
While many older adults do just fine with a regular consumer-grade tablet, others do better with a “senior tablet,” which has safety precautions and a simplified interface. Learn what to look for if you are considering one for your relative.


While many older adults do just fine with a regular consumer-grade tablet, others do better with a “senior tablet,” which has safety precautions and a simplified interface. Learn what to look for if you are considering one for your relative.

Providing comfort and calm is the watchword for the day of travel with a person who has dementia. Take advantage of the help that is available from airport personnel.

Failure to follow medical advice is one of the primary reasons older adults end up in the hospital. What can you do to help your loved one adhere to the doctor’s orders?

If your loved one has COPD, it’s important to understand which foods are most helpful and which should be limited. You might be surprised by the difference nutrition can make!

As a family caregiver, it’s easy to put your own needs last. You may feel it is a virtue, but actually, you are putting yourself and your loved one at risk. You simply have to take breaks and to safeguard your own well-being. Caregivers who don’t experience significant mental and physical health consequences.

How to pay for care is a big worry for families. Learn about options for financial support, as well as tax and workplace protections to assist you as the family caregiver. There are also legal documents your loved one will need to prepare to be sure their wishes are followed. For that, it’s best to work with an attorney.

November is National Family Caregivers Month. Whether you are new to family caregiving or have been doing it for a while, we outline the top strategies that will help you navigate the process effectively and keep stress to a minimum. This week we focus on gathering information and finding help.

November is COPD Awareness Month (chronic obstructive pulmonary disease). If your loved one has respiratory problems and needs oxygen, they can still travel by plane. You just need to plan ahead.

Perfectionism is a mental habit that can get in your way as a family caregiver. Your intentions are the best, for everyone. But it will be better for you, and your loved one and family, if you can develop a more nuanced approach where doing the best you can REASONABLY do is the gold standard.

Many families instinctively feel that the amount of money spent on a funeral reflects the love felt for their departed relative. Not so! That belief can result in unnecessary debt. Consider separating the disposal of the body from the memorial service and focus on what will be the most personally meaningful for survivors.

Pain is no fun, whether in a knee, a neck, or elsewhere in the body. There are drugs that dull pain. But they don’t cure the problem. Plus, prescription drugs usually have side effects or are addictive. Physical therapy (PT) is a proven treatment that can relieve pain and in some instances, cure the problem.

Perhaps you wonder if your family member is a “hoarder.” (You may even harbor secret fears about yourself!) We all have cherished possessions. From trophies to teacups. Spare buttons to cans of half-used paint. But hoarding is different.

Does your loved one need to downsize? Move? Does the prospect seem overwhelming? Perhaps not just physically, but emotionally too? Enter the senior move manager: Part mover, part interior decorator, part compassionate friend. These professionals take a holistic approach. They handle the physical logistics. They are also skilled at assisting older adults with the emotional side of a move.

This is World FTD Awareness Week. People with FTD often exhibit sudden changes in behavior or personality. FTD is frequently misdiagnosed as Alzheimer’s disease, depression, or some psychiatric disorder. It is the most common form of dementia for people under 65 (early-onset dementia).
National Stepfamily Day falls in September. To honor these special families, we are featuring an article about working with stepsiblings. It could be that you have hardly met your “brothers and sisters,” yet you may be called upon to work together in an eldercare crisis.

September is Pain Awareness Month. Consider addressing your loved one’s pain with tips from music therapy. No drugs. No side effects. Simply drawing on the mind-body connection to lift mood, enhance relaxation, and distract from pain.

A difficult or abusive childhood makes for a very uncomfortable caregiving situation when your parent begins to need help in their later years. You don’t have to do it all. Consider these strategies for doing what feels right while also taking care of yourself.

Support your loved one’s independence with simple but important low-vision adaptations in the bathroom: Color contrasts, a magnifying mirror, a shower caddy, etc.

The U.S. Surgeon General reports we have a loneliness epidemic. Like smoking and obesity, social isolation creates a greater risk for poor health. It’s been associated with a 48 percent increase in “premature death” (a death where a change in lifestyle could have resulted in a longer life). Our social health affects our physical health.

It will likely take one to three months for you and your loved one to get used to the new living situation at memory care. Strong emotions are to be expected. But there are strategies to ease the transition and promote a resilient recovery for both of you.

Have you spent years encouraging a loved one to steer clear of salt or avoid fat? There is no doubt that a healthy diet can promote longevity. But there does come a time when quality of life is more important.

Is being selfish always bad? Is it possible to be too altruistic? Take the survey to see where you stand. It could be that you and your loved one would benefit from your being a little more selfish—in a healthy way.

Once you’ve decided to go, there are a few things you can do weeks ahead of time, and then while packing, that will ease many of the challenges that might arise in the course of your travels.

If your loved one is frail or has dementia but needs treatment for pneumonia, a urinary tract infection, or a flare of heart failure or COPD, you may be eligible for a Hospital at Home program. A team of professionals mobilizes to treat your relative at home. Popular in Europe, this program provides quicker recovery without the common setbacks of a hospitalization.

For Elder Abuse Awareness Month, we look at the problem of bullying and exclusion in senior housing. It’s surprisingly common. Fortunately, there are things you can do, whether your loved one is on the receiving end or the “bully” themselves.

A relative’s serious illness pushes us to communicate deep thoughts and bring closure to the relationship before we lose the chance. Don’t postpone those discussions! They may be awkward, but they can be profoundly important for all involved.
Extreme temperatures are especially hard on older adults. There are things you can do for your loved one to reduce the impact of a heat wave this summer, even if you live far away.

Are you hoping to travel this summer with a loved one who has dementia? New and crowded situations are notorious for creating confusion and outbursts. Take a moment to reflect on your relative’s likely reactions and what you can do to keep them comfortable.

June 15 is World Elder Abuse Awareness Day. There are seven different ways that elders can be exploited. Learn what they are and how to report it if you suspect a problem.

As a family caregiver, you need to take a break now and then. It’s not selfish. It’s essential! But in order to truly rest, you’ll want to be sure your relative is covered.

National Cancer Survivors Day is coming up (June 4), which celebrates the fact that 66% of those ever diagnosed with cancer are still alive five years later. Help your loved one get a jump on any potential cancer by taking advantage of these free screening tests.

Nearly one in four older adults experiences ringing in the ears, called “tinnitus.” For some, it interferes with concentration and is so severe it leads to insomnia, depression, and anxiety. In honor of Better Hearing and Speech Month, we highlight what you can do to help your loved one address this all-too-common condition.

Once you decide memory care is the wisest path, the next step is choosing a facility and creating a smooth moving day. Many memory care communities have a “move-in coordinator” or other family liaison. Rely on this professional for guidance.

A long-time hospice nurse—someone deeply committed to caring for the seriously ill—created this list of the top five deathbed regrets she frequently observed in her patients. She vowed to take these lessons to heart. Do any of these ring true for you?
If your loved one is admitted to a skilled nursing facility, Medicare requires the staff develop an initial, personalized care plan within the first 48 hours. This describes who should be doing what. Then, within the first 14 days, the staff must assemble a comprehensive assessment, which must include your loved one’s needs and strengths.

It’s important to do the best you can when caring for a loved one. But aiming for perfection can bring on problems. For yourself, in terms of anxiety, depression, and low self-esteem. And for your relative and other family members, who may feel burdened by living under the stress of constant measurement and judgment.
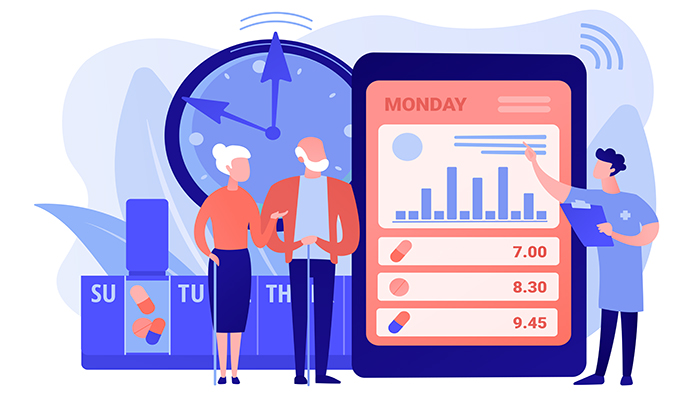
For many people, a pillbox is just the ticket. But as we age, we may take more medicines. Filling the box requires more concentration. Remembering to take the meds can become more challenging. Many families turn to technology to help an aging loved one.
If you are the person most likely to step in if your loved one is unable to get to the bills—a hospitalization, dementia—you need to get oriented. And organized! It’s easy to lose track of paperwork, especially someone else’s. Professionals recommend gathering important documents in a file or binder for safekeeping. Put that in a locked and fireproof location. Consider a small home safe. Or a safe deposit box at the bank.

April 10 is Siblings Day! How are things going with your siblings? Does everyone in your family participate in the care of your loved one? Is there agreement on the problems? The solutions? If not, you aren’t alone with this issue. But you could probably use a family meeting or two to get everyone rowing in the same direction.
If your spouse is younger than 65 and has received an Alzheimer’s diagnosis, you may feel in a world all your own. You probably don’t know anyone else in this situation and may sense a social stigma. It can be scary. Lonely. And feel just not fair!

Did you know “false teeth” need to be brushed daily, just like “real teeth” do? Learn how you can help your loved one avoid infections, maintain good nutrition, and extend the life of their dentures.

Food is so profoundly linked to health and love, it can be distressing to realize that someone you care for is missing meals or otherwise eating poorly. There are many services available to help, each with their own special procedures. Learn about the questions you’ll want to ask.

People with moderate dementia are rarely aware of their need for help. It will be the family members who make any placement decisions. How do you know when this option should be explored?

If someone else in your family has primary responsibility for the care of your loved one, that doesn’t mean you don’t have anything to contribute. Far from it! Caring for an older adult is more than one person can do alone. There are many ways to lend a hand (even if you don’t live nearby).

February is Heart Month. If your loved one needs frequent naps and gets out of breath easily, he or she may need a daily life energy budget. (This is especially true for people with heart failure.)

If the person you care for has a low vision diagnosis, three types of modifications to the home can make life easier: Lighting, glare control, and the use of color contrast. Fortunately, these strategies are relatively inexpensive.

Frustrated in your search for a paid caregiver? You are not alone. There is an extreme shortage of helpers right now. Even before COVID, the demand for aides was greater than the supply. The “Great Resignation” hit the caring professions hard. Caregivers close to retirement left early. And many younger workers decided to opt for safer, less demanding jobs. In some states, as many as 38% of direct-care workers chose other occupations last year.

Caring for a parent long distance brings its own challenges. With planning, organization, and frequent communication—plus a little help from technology—you can provide effective support.

Catching things early is big with Medicare. Every year, all Medicare enrollees are eligible for a free “Wellness Visit” with their primary care doctor. This is NOT an annual physical, so don’t use that term when making the appointment. Beyond basic vitals—height, weight, blood pressure, and pulse—there is no physical examination. If a physical exam is done, your loved one may have to foot the bill.

Being primary can be quite a job. In many cases it involves driving to the doctor and managing medications, handling finances, providing for daily needs, coordinating care services, and keeping the elder’s spirits up. If you are that person, don’t try to do it alone—even if it seems like that’s the only choice.

Our eyes show us the world. If something goes wrong with them, it can affect our total well-being. Dry eye syndrome makes eyes feel gritty, burning, itchy, and sensitive—discomforts that are hard to ignore! It typically manifests with age and affects as many as 30% of older adults.

The dangers of cold weather are obvious outdoors. But there are dangers indoors, too, most often because the house thermostat is set too low. People can die from being too cold. Older adults are especially at risk.

Take any roomful of people and likely two-thirds of them have relatives who aren’t talking to each other. Families are messy. Hurts abound. Some people wait until a serious diagnosis to reconcile. They often regret the years of separation they can never retrieve. Others try forgiveness earlier in the process. There’s no right or wrong.

The grandparent–grandchild relationship can be precious, like no other. But even young children notice if Grandma or Grandpa isn’t acting the way they used to, or the same way others do. And they will have questions.

If you expect older visitors this season, check your home for hazards. Older adults often have impaired balance and vision. This makes them prone to falling, especially in new surroundings. And fragile skin and bones can mean double trouble if someone does take a spill.

Taking the right medicines at the right time is extremely important to health management. But 75%–96% of older adults admit that they frequently make mistakes with their medication. Is your loved one among them?

Deciding what holiday gifts to give a person with memory loss can be challenging. From seasonal activities to digital picture frames or fuzzy robo-pets, we’ve got suggestions!

November is National Family Caregivers Month. We want to express our gratitude to you, who are part of the 40 million people (one in six Americans) who care for an older adult friend or relative. So many family caregivers feel invisible, we thought we’d give you some perspective on the scope of family caregiving across the country.

Are frequent visits to the ER a significant part of the past six to twelve months? Does your loved one seem more fatigued? Less interested in eating? Perhaps a bit withdrawn? These symptoms may be hallmarks of a serious illness your relative will overcome. But it’s also possible that these signal that your family member no longer has the reserves to beat their condition.

If the person you care for is a veteran and is seriously ill, they may qualify for a VA program designed to control symptoms that cause pain, discomfort, or mental or emotional distress. Called “palliative care,” this program is available even if the problems are as a result of treatments, not just the medical condition itself.

Do you ever wish you could wave a magic wand for more joy? Patience? Optimism? Motivation? Maybe less irritability and stress? It’s actually accessible now, no wizardry required. Just a shift in attention. Welcome to “anticipation.”

The most common form of dementia is Alzheimer’s disease. However, there are many other conditions that also bring on memory problems. It is important to accurately identify the cause, even if there’s no cure, because this will shape the best strategy for addressing difficult symptoms.

It’s unpleasant to imagine that your loved one might become the victim of crime, but it’s worth considering. There are valuable preventive steps to take. Unless your relative lives in a high-crime neighborhood, their greatest risk is a property crime in or around their home.

If your loved one is discharged from the hospital to a skilled nursing facility (SNF), their care will be in the hands of a team of specialists. It’s a good idea to understand the players’ roles so you know whom to call upon for what.

Depression is common in older adults. It’s long been known that brisk exercise can help reduce depression. But it turns out that exercise doesn’t have to be vigorous to make a difference. Even mild exercise can be effective.

No one likes to dwell on the possibility of disaster. But we all need to prepare for one, just in case. Help your relatives gear up for safety. Whether you live across town or across the nation, the action items are the same.

If your loved one has balance problems, the culprit may be in the medicine. Many common medicines have side effects that can impair balance and lead to a fall. Over 40% of persons age 65 and older take five medications or more. This increases the chance that at least one of the drugs has side effects of dizziness, blurry vision, drowsiness, or muscle weakness.

Has your parent remarried? If so, you may be sharing the caregiving with a person you don’t know very well. Biological families often encounter tensions when it comes to eldercare. Add a stepparent and the challenges can grow exponentially.
Medicare pays for many screening exams, and even counseling sessions, to help nip common illnesses in the bud. Screening tests are designed to identify problems before symptoms emerge. They are usually for people who are considered to be “at risk” for getting a specific disease. Here are some of the most common noncancer preventive services that Medicare covers. Ask the doctor if your loved one should be tested.

Good communication requires both speaking and listening. Oddly enough, if you make a specific effort to listen, it can open doors. Once “heard,” the other person may be more willing to hear your point of view. Deep listening is more difficult than it sounds. It’s not passive. It requires concentration. It also takes humility and empathy.

For a teen, a relative’s dementia can turn a close relationship into one that’s now awkward, confusing, and embarrassing. And creates feelings of guilt.

After you have scoured the Internet to help your relative find a potential new doctor—someone on their plan and with no obvious red flags—it’s time to get more specific. The doctor’s website may provide some descriptive information, but most likely, you’ll want a conversation.
For most family caregivers, frustration and guilt are common, as is anxiety and resentment. These feelings are normal and reasonable under the circumstances. It’s not realistic to eliminate negative emotions. Caring for an ailing family member IS emotionally taxing, especially in the case of memory loss. But sometimes the negativity can feed on itself.

Even pre-COVID, many 90-year-olds adamantly refused to go to a senior center, saying they didn’t want to be around “all those old people.” (!) Does this sound like your loved one? Admittedly, the senior centers of the past tended to focus on bingo and crafts. These activities are of limited interest to the newest generation of older adults. Happily, senior centers have been updating. Bingo and crafts are still there. But the upswing in technology use during COVID catapulted many centers into the 21st century

With summer’s warm weather, be on the lookout for dehydration in your loved one. The signs include confusion, fatigue, weakness, and sleepiness. Some people become dizzy and their balance is thrown off. Dry mouth, headaches, and muscle cramps are other symptoms of dehydration.

If the person you care for has dementia—memory or thinking problems from a condition such as Alzheimer’s, a stroke, or Parkinson’s—unpaid bills or a messy checkbook may have been your first sign that something was amiss. Certainly, in the later stages of dementia, your loved one won’t be able to manage their finances. But what about the in-between?
Elderly parents are living longer. Children are often dependent for more years than expected. Add to this the ongoing responsibilities to spouse/partner and jobs, and there is little wiggle room for the millions of family caregivers who find themselves squeezed in the middle as the “Sandwich Generation.”

Many older adults experience swollen legs and feet. For some, it’s because of sitting a lot and leading a sedentary lifestyle. For others, it’s the water retention side effect of a medication. And for others, the swelling—called “edema”—is a symptom of a chronic or even serious illness such as heart failure or liver or kidney disease.
© 2002-2024, LionHeart Eldercare & Consulting. Site created by Elder Pages Online, LLC.